Healthwise
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Endometriosis
Condition Basics
What is endometriosis?
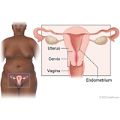
Endometriosis (say "en-doh-mee-tree-OH-sus") occurs when cells that are like the cells that line the inside of your uterus grow outside of your uterus. These cells form clumps of tissue called implants. They usually grow on the ovaries, the fallopian tubes, the outer wall of the uterus, the intestines, or other organs in the belly. In rare cases, they spread to areas beyond the belly.
Endometriosis usually isn't dangerous. But it can cause pain and other problems.
What causes it?
Experts aren't sure what causes endometriosis. Problems with reproductive organs may cause endometrial cells to go up through the fallopian tubes and into the belly. And your immune system may not kill these cells outside the uterus like it should. These cells might be carried through the body by blood or lymph fluid.
What are the symptoms?
The most common symptoms are pain, bleeding, and trouble getting pregnant. You may have pain in your lower belly, rectum or vagina, or lower back. And you may have heavy periods, bleeding between periods, bleeding after sex, or blood in your urine or stool. Symptoms often are most severe before and during your menstrual period.
How is it diagnosed?
Your doctor will ask questions about your symptoms, periods, past health, and family medical history. You may also have a pelvic exam. And you may have imaging tests, such as a pelvic ultrasound or MRI. But to find out for sure if you have endometriosis, a surgery called laparoscopy is often used.
How is endometriosis treated?
Treatment choices depend on whether you want to control pain or you want to get pregnant. For pain and bleeding, you can try medicines or have surgery to remove the endometrial tissue and scar tissue. If you want to get pregnant, you may need surgery to remove the endometrial tissue.
Cause
Experts don't know what causes endometriosis. But they do know that the hormone estrogen makes the problem worse.
Here are some possible causes.
- Your immune system may not get rid of endometrial cells outside of the uterus like it should.
- Abnormal structure of the uterus, cervix, or vagina may cause too many endometrial cells to go up through the fallopian tubes and then into the belly. (This is called retrograde menstruation).
- Blood or lymph fluid may carry endometrial cells to other parts of the body. Or the cells may be moved during a surgery, such as a cesarean delivery.
- Cells in the belly and pelvis may change into endometrial cells.
- Endometrial cells may have formed outside your uterus before you were born.
- Genetics. Endometriosis can run in families.
What Increases Your Risk
Your risk of endometriosis is higher if:
- You are between puberty and menopause (around age 50).
- You have a family history of endometriosis.
- Your menstrual cycles are less than 28 days.
- Your menstrual flow is longer than 7 days.
- You started menstruation before age 12.
- You have never been pregnant.
- Your uterus, cervix, or vagina has an abnormal shape that blocks or slows menstrual flow.
Symptoms
Sometimes endometriosis does not cause symptoms. But when symptoms are present, they can range from mild to severe. Symptoms may include:
- Pain. You may have:
- Pelvic pain.
- Severe menstrual cramps.
- Low backache.
- Pain during sexual intercourse.
- Rectal pain.
- Pain during bowel movements.
- Trouble getting pregnant (infertility). This may be the only sign that you have endometriosis.
- Abnormal bleeding. This may include:
- Heavy periods or bleeding between periods.
- Vaginal bleeding after sex.
- Blood in the urine or stool.
Symptoms are often most severe just before and during your menstrual period. They may get better as your period is ending. But sometimes pain occurs all the time.
What Happens
Your uterus is lined with tissue called endometrium. When you have endometriosis, clumps of similar tissue (called implants) form outside your uterus. The implants can be painful. Sometimes they form scar tissue or fluid-filled sacs (cysts). Scar tissue may make it hard to get pregnant.
Learn more
When To Call
Call a doctor now if you develop sudden, severe pelvic pain.
Call your doctor if:
- Your periods have changed from relatively pain-free to painful.
- Pain interferes with your daily activities.
- You start to have pain during intercourse.
- You have pain when you urinate, have blood in your urine, or can't control the flow of urine.
- You have blood in your stool, you develop pain, or you have a significant, unexplained change in your bowel movements.
- You are not able to become pregnant after trying for 12 months.
Check your symptoms
Exams and Tests
To find out if you have endometriosis, your doctor will ask questions about your symptoms, periods, past health, and family history. (It sometimes runs in families.) You may also have a pelvic exam. And you may have imaging tests, such as a pelvic ultrasound or MRI, to look at the organs in your belly.
Your exam, symptoms, and risk factors may strongly suggest that you have endometriosis. But the only way to be sure that you have it is to have surgery. Laparoscopy is often the surgery used. During this surgery, the doctor puts a thin, lighted tube through a small cut in your belly. This lets the doctor see what's inside your belly.
Learn more
Treatment Overview
Treatment depends on how much pain you have and whether you want to get pregnant. Treatments include:
- Over-the-counter pain medicines like ibuprofen (such as Advil or Motrin) or naproxen (such as Aleve). These can reduce bleeding and pain.
- Hormone therapy. This can help reduce pain and menstrual bleeding. It can include hormonal birth control and other medicines.
- Laparoscopy to remove growths and scar tissue. This may reduce pain, and it may help you get pregnant.
A hysterectomy and oophorectomy (removal of the uterus and ovaries) are sometimes used as a last resort for severe pain.
If you're close to menopause, you may consider treatment with medicines rather than surgery. Endometriosis usually stops causing problems when you stop having periods.
Learn more
Self-Care
Home treatment may ease the pain of endometriosis. You can try the following things along with your other treatments.
- Apply heat to your lower belly.
Use a heating pad or hot water bottle, or take a warm bath. Heat improves blood flow and may relieve pelvic pain.
- Relieve back pressure.
Lie on your back and place a pillow under your knees. Or lie on your side and bring your knees up to your chest.
- Use relaxation techniques and biofeedback.
- Exercise regularly.
Exercise improves blood flow, increases pain-relieving endorphins naturally made by your body, and reduces pain.
Explore more
Medicines
Hormone therapy (HT) can often relieve the symptoms of endometriosis. It can be used to reduce pain and bleeding. It may also shrink endometriosis growths (implants) and keep them from spreading.
HT prevents pregnancy, so it's not a good option if you want to get pregnant soon.
What are the types of HT?
Estrogen-progestin therapy plus a nonsteroidal anti-inflammatory drug (NSAID) are often used if symptoms are mild to moderate. If you have severe symptoms, or if estrogen-progestin therapy and NSAIDs don't relieve your symptoms, you may have other HT options. Talk to your doctor about the benefits and risks of the different types of HT.
- Estrogen-progestin therapy (birth control pills, patch, or ring) may reduce painful periods. It's less likely to cause serious side effects than other hormone treatments. It can often be used continuously for years, until pregnancy is desired or until the age of menopause. It is often used with NSAIDs. These include prescription medicines and over-the-counter NSAIDs, such as ibuprofen (Advil, Motrin) or naproxen (Aleve).
- Progestin-only therapy stops ovulation and lowers estrogen. It usually shrinks implants and reduces pain. Progestins are given as a shot or a pill. Or you may use the levonorgestrel intrauterine device (IUD).
- Gonadotropin-releasing hormone (GnRH) therapy lowers estrogen. It triggers a state that's like menopause. This shrinks implants and reduces pain in most cases. GnRH therapy can have more side effects than some other types of HT.
- Danazol therapy lowers estrogen levels and raises androgen (male sex hormone) levels. It triggers a state that's like menopause. It may shrink implants and reduce pain for several months after treatment. But danazol can have a lot of side effects.
How can you decide if you should take HT?
You might consider taking HT if:
- Your symptoms are mild to moderate.
- You don't want to get pregnant soon.
- You are close to menopause. Your estrogen levels will drop when your menstrual periods end. And you will probably stop having endometriosis symptoms.
You might decide not to take HT if:
- You want to get pregnant soon.
- You can manage your pain with other treatments.
- You want to avoid the possible side effects of HT.
Your doctor can help you weigh the pros and cons of HT so you can decide what's right for you.
Surgery
Surgery may be recommended when:
- Treatment with hormone therapy has not controlled symptoms, and symptoms interfere with daily living.
- Endometrial growths or scar tissue interferes with other organs in the belly.
- Endometriosis causes infertility.
Surgery choices include:
- Laparoscopy. This is the most common procedure for treating endometriosis. It is used to look for and possibly remove growths and scar tissue. It can help relieve pain and can improve the chances of pregnancy for some people. But the pain can come back.
- Hysterectomy with oophorectomy. This surgery removes the uterus and ovaries. It's used only when you have no plans to get pregnant and have had little relief from other treatments. It can help with pain for the long term. It causes early menopause.
Learn more
Related Information
Credits
Current as of: May 5, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: May 5, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.